Drive north from the bustling University of Maryland Medical Center (UMMC) in downtown Baltimore and in minutes you’re in the heart of the city’s Mondawmin neighborhood. Rich in African American history, Mondawmin is better known today as the epicenter of the riots that struck Baltimore after the death of Freddie Gray. Mondawmin’s considerable challenges include poverty, underemployment, violence, drug abuse, crime, substandard housing, and a host of health inequities.
Seeking solutions to one of those inequities—poor birth outcomes—the University of Maryland (UMD) Schools of Medicine and Social Work are partnering with the Mondawmin community, leveraging local expertise and assets to help improve health services and conducting research to measure the impact of the intervention on the underserved population.
Simultaneously, a team from the University of Kentucky College of Medicine is also putting implementation science into practice. Implementation science is the study of approaches that integrate research findings into health care practice. The team is training health professionals, particularly in rural clinics, in better techniques for lung cancer screening. Kentucky leads the country in lung cancer incidence and deaths.
Both projects won grants in a 2015 competition, Advancing Implementation Science in Community/Academic Partnered Research, sponsored by the AAMC and funded by the Patrick and Catherine Weldon Donaghue Medical Research Foundation. The grants are part of the AAMC Accelerating Health Equity, Advancing through Discovery (AHEAD) initiative, which supports member institutions in implementing and evaluating practices that can improve community health and reduce health inequities.
Improving birth outcomes
To improve birth outcomes in Baltimore, UMMC partnered with B'more for Healthy Babies (BHB), a community group that supports women and their partners during pregnancy. UMMC sends staff to schools, barbershops, a shopping mall, and other anchors of community life to provide information and guidance about breastfeeding, smoking cessation, and safe sleeping for infants. The grant enabled UMMC to expand its services to BHB.
“Our goal is to improve birth outcomes. But we realized that we can’t just be doing it within the medical system. We have to go into neighborhoods to be where pregnant women are and work with them there.”
Wendy Lane, MD, MPH
University of Maryland School of Medicine
As part of the partnership with BHB, UMMC staff reach out to teens and parents at Frederick Douglass High School, the alma mater of Thurgood Marshall, the first black justice of the U.S. Supreme Court, which is just blocks from a CVS pharmacy that was destroyed during the 2015 riots. Myron Missouri, from the UMD School of Social Work, serves as resource dad/community outreach worker at the school. He counsels teen parents and provides referrals for childcare, job training, mental health counseling, and other social services. UMMC also supports an office in nearby Furman L. Templeton Preparatory Academy, where two lactation experts teach new mothers how to breastfeed and connect with social services.
“From a big picture perspective, our goal is to improve birth outcomes. But we realized that we can’t just be doing it within the medical system,” said Wendy Lane, MD, MPH, an associate professor of epidemiology, public health, and pediatrics at the University of Maryland School of Medicine and the principal investigator for UMMC’s work with BHB. “We have to go into neighborhoods to be where pregnant women are and work with them there to figure out what they want and what they need in order to improve birth outcomes.” Long term, the program seeks improvements in maternal health during pregnancy, a reduction in preterm births and neonatal intensive care, and lower hospital costs.
Early results are promising. In one study of a cohort of women who delivered babies at UMMC, initial baseline data compiled in late 2015 showed just 31% successfully started breastfeeding. After staff education and other interventions, that total jumped to 41% by early 2017. That’s still shy of the Joint Commission benchmark of 52%, “but we’re getting there,” said Monika Bauman, MS, BSN, RN, patient care services director for women’s and children’s health at UMMC.
“This program provides tremendous opportunities for our students, residents, and trainees to become directly involved in improving the health of people in our nearby neighborhoods and deliver much needed services to the areas of the city that are facing the greatest health challenges,” said E. Albert Reece, MD, PhD, MBA, vice president for medical affairs at the University of Maryland and the John Z. and Akiko K. Bowers Distinguished Professor and dean at the University of Maryland School of Medicine. Residents at UMMC, for instance, receive three hours of training on breastfeeding advantages and issues, and two residents in pediatrics created an elective that leads to lactation consultant certification. Medical students also go into Baltimore communities to conduct research and help deliver community services.
Mohan Suntha, MD, MBA, president and CEO of UMMC, echoed the importance of the effort. “Extending ourselves into our community, having a presence outside the walls of our organization, and understanding the unique needs of our local community” is a fundamental responsibility of UMMC, he said. A new UMMC community engagement center reflects the commitment of UMMC’s board to invest in community outreach and serve as an anchor institution in Baltimore, he added.
Implementation science in Appalachia
Drive 60 miles northeast of the University of Kentucky (UK) College of Medicine and it’s not long before verdant horse farms give way to more hardscrabble terrain. There, where the foothills of the Appalachian Mountains begin to take form, clinics in rural towns such as Frenchburg and Olive Hill are on the front line in addressing lung cancer, opioid abuse, and Kentucky’s other entrenched health problems.
In an implementation project based on earlier formative community-engaged research, UK HealthCare principal investigator Roberto Cardarelli, DO, MPH, and colleagues partnered with the St. Claire Regional Medical Center (SCRMC) in Morehead, Kentucky, to train health providers and staff on how to improve practices in tobacco cessation education and early screening for lung cancer.
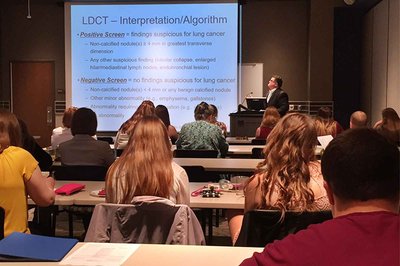
With support from the Northeast Kentucky Area Health Education Center, the project also educates a spectrum of learners at SCRMC’s main campus. Periodic symposia are offered for regional health professionals, and additional education is provided to students in the UK satellite medical school at SCRMC and to residents, nursing students, and future physician assistants.
“Our mission has always been to use implementation science to improve community health,” said Kevin Pearce, MD, MPH, professor and chair of family and community medicine and associate dean for rural and community health at UK College of Medicine. “The timing is right for this project because we found that guidelines for cancer screening were not in [providers’] heads or in their practice yet.”
Very early data show mixed results—an increase in low-dose computed tomography tests ordered at one clinic is offset by declines in such orders at another clinic. But Cardarelli and colleagues take the long view and remain convinced that as they tweak and expand their work they will see gains.
“It’s not community engagement unless you are really engaging the community as a partner. That’s a basic tenet of what practice-based research is all about.”
Kevin Pearce, MD, MPH
University of Kentucky College of Medicine
Cardarelli gets high praise for his ability to develop a real partnership with a community hospital and clinics. “If you really want to develop these types of projects, you have to develop rapport with the folks who are going to carry them out,” said Greg Bausch, PharmD, vice president and COO of the St. Claire Medical Group. “Roberto understands that implicitly. He makes time to come out and work with us, and he’s here a couple of times a month. I think that makes all the difference.”
One of the distinguishing features of Kentucky’s project is that most of the funding for it goes directly into the community, said Pearce. Further, the project team has avoided the pitfall of not listening carefully to its partners. “It’s not community engagement unless you are really engaging the community as a partner,” Pearce stressed. “That’s a basic tenet of what practice-based research is all about.”
The initiatives of UMMC and UK HealthCare demonstrate the value of community partnerships, summed up Philip M. Alberti, PhD, AAMC senior director of health equity research and policy. “These initiatives, made possible by the Donaghue Foundation, exemplify what it means for academic medical centers to listen to the people they serve, take the time to respond in culturally relevant ways, and integrate local wisdom and scientific evidence into systems and initiatives that minimize inequities in health and health care.”
