With the possible exception of a priest’s clerical collar, there is no workplace clothing as threaded with symbolism as a doctor’s white coat. Trained surgeons, soon followed by physicians, began wearing white lab coats in the late 1800s to distinguish themselves from the quacks and snake-oil healers who did not practice evidence-based medicine.
These days, depending on who you ask, the white coat might stand for professionalism, integrity, and the highest commitment to caring for the sick and suffering. Or it might represent elitism and the reckless spreading of germs.
While 97% of medical schools have a white coat ceremony, the use of the white coat in clinical settings varies considerably between institutions and specialties. Pediatricians and psychiatrists have been more vocal about avoiding them, for example, in part because patients find them threatening. The Mayo Clinic instructs its physicians to wear business attire only, citing a need to break down the barrier between physicians and patients.
Now, in the largest study of its kind, researchers at the University of Michigan surveyed 4,000 patients at 10 U.S. academic medical centers and found that a physician’s clothing affects how patients view their doctor, as well as how satisfied they are with their care. Physicians who wore a white coat over business attire (navy blue suit and dress shoes) were deemed more knowledgeable, trustworthy, caring, and approachable, particularly by patients 65 and older. Doctors who wore scrubs with a white coat scored next highest, followed by those in business attire with no coat. Some exceptions: In both operating and emergency rooms, more patients preferred doctors in scrubs only.
“What we wear is such an easy thing to modify,” says Christopher Petrilli, MD, assistant professor of hospital medicine at the University of Michigan Medical School and lead author of the study. “At a time when we’re all trying to be more patient-centered, doesn’t it make sense to do what people want?”
Image versus infection
Not everyone is on board with the white coat, though. “Asking patients what they want doctors to wear isn’t even a valid question,” says Mike Edmond, MD, chief quality officer and clinical professor of infectious diseases at University of Iowa Hospitals and Clinics. “No patient picks their doctor that way.”
He recalls wearing jeans to work one day early in his career, “because I’d just be doing paperwork. A patient needed me, so I apologized for not being in my ‘doctor clothes.’ He said, ‘I don’t care if you are in your pajamas. I just want you to help me.’”
Besides, Edmond points to the robust evidence that white coats harbor potentially dangerous microbes, especially around the cuffs and pockets. Following an initial study in the United Kingdom in 1991, numerous other researchers have confirmed how germy white coats can be. By 2007, the BBC pronounced white coats as more or less dead. And in 2008, Britain’s National Health Service, which had already discouraged white coats because they created a barrier between patient and physician, insisted that those who chose white coats must be bare to the elbows. By 2009, the American Medical Association even toyed with the idea of banning white coats in hospitals.
Some argue that white coats might be safer if doctors laundered them more often. While almost everything else that comes in contact with a patient is sanitized or tossed, doctors typically wash their lab coats once every 12 days and only 70% of physicians admitted to ever laundering their neckties.
Some infection specialists, while acknowledging that there is no evidence yet to support the idea that all these white coat germs are making patients sick, say the answer is simply to roll up the sleeves. A 2017 study, led by Amrita John, MD, an infectious disease specialist at University Hospitals Cleveland Medical Center, showed that long sleeves cause cross-contamination.
Her team had 34 health care workers wear coats with both long and short sleeves. First, they examined a dummy contaminated with DNA from the cauliflower mosaic virus and then one that wasn’t. (Harmless to people, the virus is similar to more destructive pathogens.) With long sleeves, 25% of the workers wound up with contamination on their coats. And 5% of the long-sleeved coats transferred the bugs to the clean dummies.
John’s stance on white coats is middle of the road. “In my medical school training in India, we didn’t want to have a barrier between patients and us. But it’s true many people expect doctors to wear them.” As a compromise, she supports wearing short-sleeved coats. “In medical school, we wore short sleeves because of the weather. Now, it’s because I don’t want to transmit pathogens.”
“In my medical school training in India, we didn’t want to have a barrier between patients and us. But it’s true many people expect doctors to wear [white coats].”
Amrita John, MD
University Hospitals Cleveland Medical Center
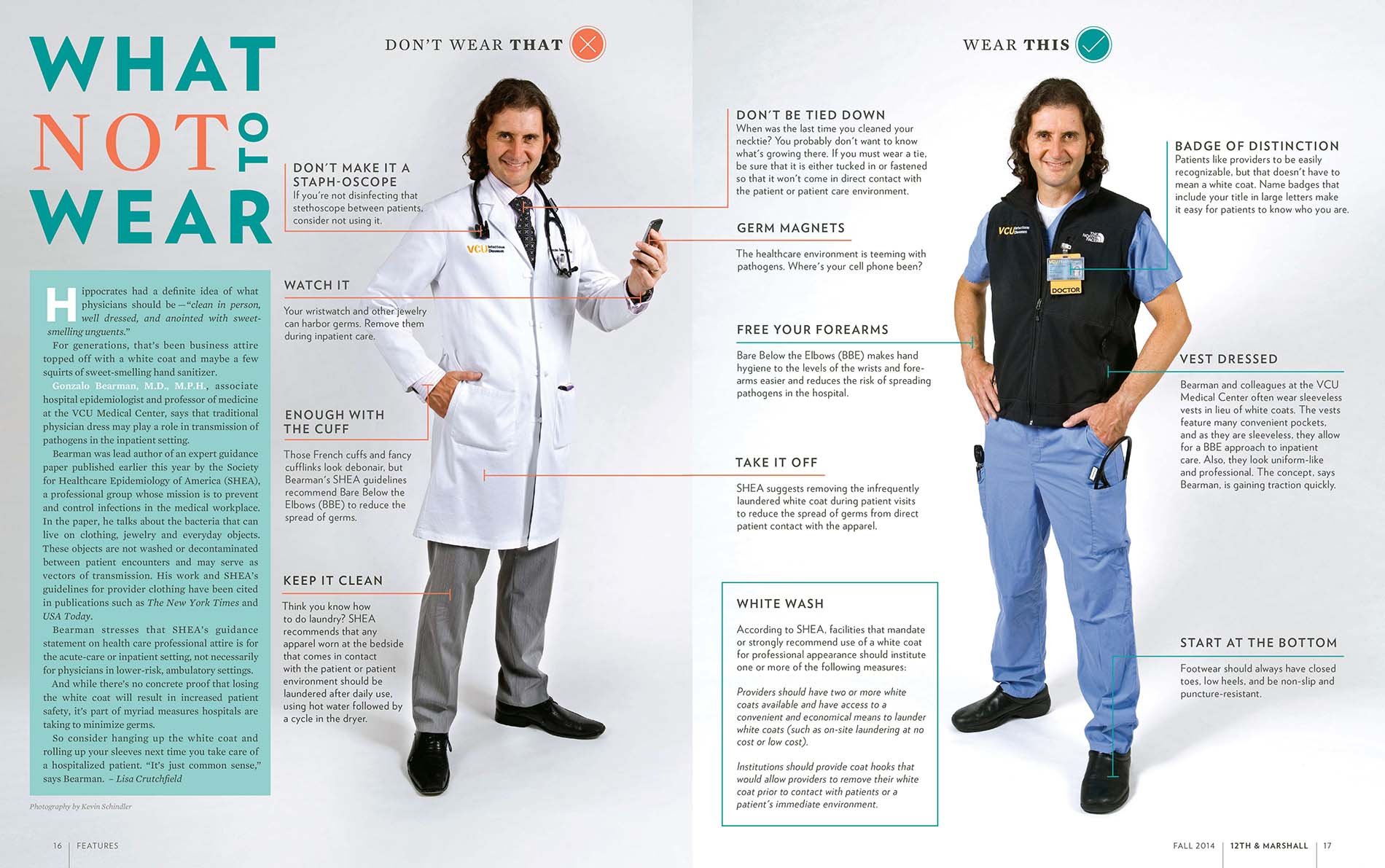
Virginia Commonwealth University School of Medicine has been out front in this area, providing doctors with a sleeveless black neoprene vest, which serves many of the practical needs of having a white coat without any of the infection risks, says Gonzalo Bearman, MD, chair of the division of infectious diseases.
With plenty of pockets, the vest keeps doctors warm but doesn’t restrict movement. “We chose black because the university’s colors are black and gold,” he says. “And we’ve now got between 70 to 80% compliance with bare-below-the-elbows, without a hard mandate. There’s no evidence this reduces infections,” he says, “but it’s a common-sense intervention.”
White coat alternatives may also help with the century-old “white coat syndrome.” First documented in 1896, experts have long known anxiety about doctors can cause high blood pressure readings in as many as 30% of patients. And new research says it’s dangerous to write white coat syndrome off as benign: A mortality study found the risk of death is twice as high for patients with white coat hypertension as it is for those with normal blood pressure.
Rethinking the medical training hierarchy
For first-year residents, white coats are short, typically hip length. Once they’ve completed that first year, they wear a longer coat, reaching toward their knees. Patients might not pick up on the difference, but insiders do. And that tradition, too, is under fire.
Osler Medical Residency Training Program at The Johns Hopkins Hospital, the country’s oldest, is abandoning its tradition of requiring first-year residents — those who have just finished medical school — to wear short white coats. These new doctors complained that it established a hierarchy that placed them beneath more experienced residents and doctors wearing long coats.
Hopkins’ short coat “stems from a unique tradition that just because you earned your MD doesn’t yet mean you are a clinician,” says Sanjay Desai, MD, director of the residency program (and a white coat fan.) “And that first year, probably the most meaningful year of a doctor’s education, is all about being a learner.”
Students interpreted the short white coat “as a physical symbol of hierarchy and rigidity, so we eliminated it. Our values haven’t changed. But I am perfectly willing to compromise on symbols.”
Sanjay Desai, MD
Johns Hopkins Hospital
But he says today’s students interpreted it “as a physical symbol of hierarchy and rigidity, so we eliminated it. Our values haven’t changed. But I am perfectly willing to compromise on symbols.”
That more egalitarian approach not only appeals to millennials, who tend to prefer more casual clothing, but also to those who believe that using coat lengths as rank gets in the way of patient safety. “The problem,” says Edmond, “is that it prevents doctors in short coats from speaking up when they see doctors in long coats about to make a mistake.”
So will the white coat vanish anytime soon? Probably not, but that won’t stop physicians from talking about it. Paul Sax, MD, an infectious disease specialist at Brigham and Women’s Hospital in Boston, says he’s taken aback by the vehement responses he gets — both pro and con — whenever he blogs about the issue.
In the end, much of it comes down to personal preference. Desai, for one, likes his white coat. “I don’t wear it every day,” he says, “but I do when I am in front of patients. It’s part of the process for me. It’s almost a uniform for when we want to help patients feel better.”