Suffering a stroke can be a devastating, life-changing event for both patients and their families, but America’s medical schools and teaching hospitals provide increasingly effective and innovative approaches to saving lives and improving quality of life after a stroke.
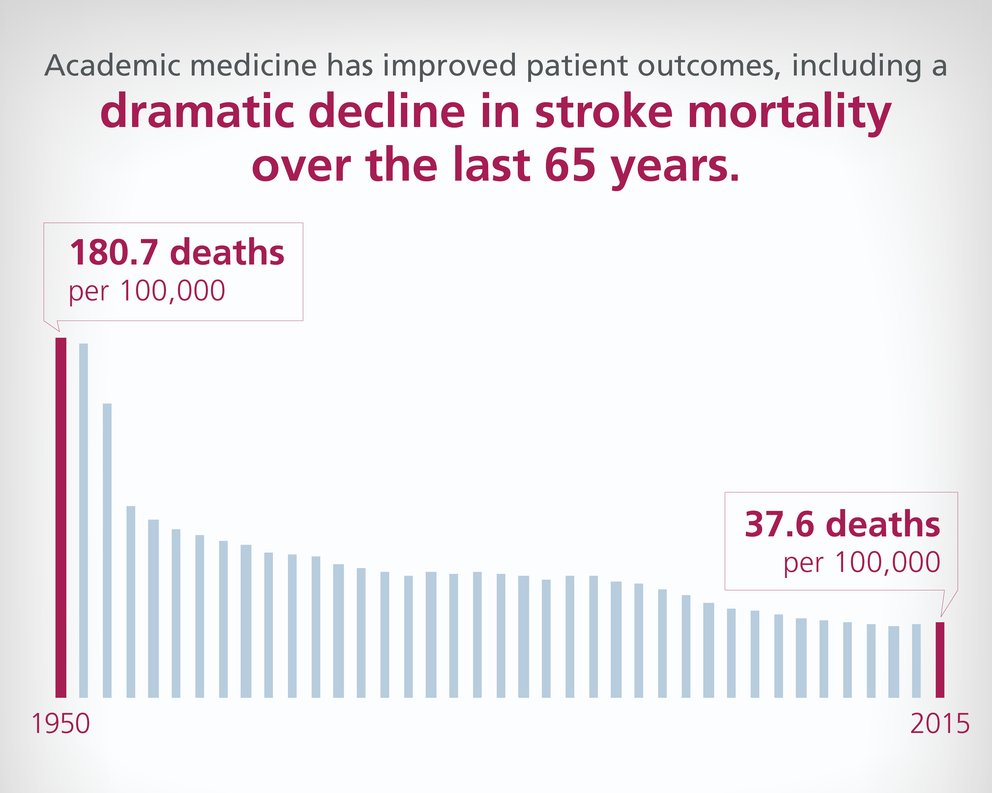
Every year, more than 795,000 people have a stroke, with about 140,000 deaths each year. The research and treatments advanced by teaching hospitals across the United States have dramatically improved the patient outcomes after a stroke including a substantial decline in death rates from 180 per 100,000 in 1950 to 40 per 100,000 in 2015.
Academic medicine’s contributions have also diminished disability rates and increased the percentage of survivors who can function independently — decreasing the staggering human and financial costs associated with stroke.
Addressing stroke through telemedicine
To diminish the physical impact of stroke in underserved areas, many of America’s teaching hospitals have partnered with facilities in rural communities to provide access to specialized care via telemedicine or teleneurology programs.
Researchers have found that some groups in rural and outlying communities comprised primarily of older persons, minorities, and those living along the so-called Stroke Belt — a 10-state region where stroke rates are higher than the general population — often lack immediate access to highly specialized stroke resources or to a general neurologist.
 National Center for Health Statistics, Health, United States, 2016 — Individual Charts and Tables: Spreadsheet, PDF, and PowerPoint files. https://www.cdc.gov/nchs/data/hus/2016/017.pdf
National Center for Health Statistics, Health, United States, 2016 — Individual Charts and Tables: Spreadsheet, PDF, and PowerPoint files. https://www.cdc.gov/nchs/data/hus/2016/017.pdf
Because “time is brain,” patients without access to specialized care are in danger of potentially losing hundreds of neurons for each hour that stroke goes untreated. Teaching hospitals provide real-time access to specialized care via two-way audio and video links and electronic access to medical records, brain imaging, and lab results. Working together with local resources, including the patient and their local clinician, teaching hospitals can:
- Help determine whether a stroke is caused by a blood clot or bleeding;
- Advise on the use of a clot-busting drug like tissue plasminogen activator (tPA) which must be administered generally within 4.5 hours of symptom onset; and
- Determine whether the patient should be transferred to a facility that has the resources to potentially perform a special radiology procedure to physically remove the blood clot.
Teaching hospitals offering telestroke/teleneurology programs
- Baylor Scott & White Health (TX)
- Emory University Hospital (GA)
- Medical College of South Carolina (SC)
- Nebraska Medicine (NE)
- Ohio State Health System (OH)
- Penn State (PA)
- Rush University Medical Center (IL)
- Stanford University (CA)
- Vanderbilt University Medical Center (TN)
- UT Southwestern Medical Center (TX)
- UCLA Medical Center (CA)
Teaching hospitals such as the Cleveland Clinic (OH), Shands Jacksonville Medical Center (FL), and MedStar Washington Hospital Center (DC) can deploy medical transport teams by helicopter, specialized land ambulance, or fixed-wing jet to speed patients to the stroke center while initiating specialized treatment during transport. Some telestroke programs are so well integrated with outlying partners that first responders notify local hospital staff and the telestroke center simultaneously when a potential stroke patient is identified, saving precious time in initiating care.
Clinical research changes stroke patients’ chances for survival and independence
In addition to technology enhancements, academic medicine has advanced research in innovative therapies for stroke patients to improve their survival rates and quality of life.
In two studies published in 2018, physician-scientists from Stanford University (CA), University of Pittsburgh (PA), and Grady Memorial Hospital (VA), reported that certain groups of stroke patients responded well to thrombectomies (surgical removal of blood clots) up to 16-to-24 hours after stroke symptoms appeared.
The studies found that patients in trials addressing certain kinds of blockages and who received “late” thrombectomies were half as likely to die and more than 3.7 times as likely to be functioning independently 90 days post-stroke compared to patients who just received the clot-busting drug tPA.
The key to the research is imaging software known as RAPID, developed at Stanford University. The software program maps dead or damaged brain tissue. Using the results from a CT scan or a perfusion MRI which shows blood flow, patients who are likely to benefit from a thrombectomy are quickly identified.
“These striking results will have an immediate impact and save people from life-long disability or death,” said Walter Koroshetz, MD, director of the National Institute of Neurological Disorders and Stroke in an NIH press release. “I really cannot overstate the size of this effect. The study shows that one out of three stroke patients who present with at-risk brain tissue on their scans improve and some may walk out of the hospital saved from what would otherwise have been a devastating brain injury.”
Specialized facilities and expert care teams
Because teaching hospitals are typically larger and tend to higher volumes of very ill and medically complex patients, they can invest in costly but important resources such as personnel, facilities, and equipment. These specialized resources improve the quality, safety, and outcomes for most medically vulnerable patients.
Teaching hospitals that specialize in stroke care and other brain or neurological disorders will often offer:
- Stroke teams. Teaching hospitals generally have a specialized stroke team, which may consist of physicians, advanced trainees (fellows) in neurology and neurointerventional radiology, nurses, and other health professionals. These teams, available 24/7 year-round, meet potential stroke patients in the Emergency Department, follow their care through discharge, and are called to the bedside for stroke-related complications.
- Neurointerventional radiology. Specially trained and certified interventional radiology physicians and advanced imaging and therapeutic equipment, available 24/7, allow stroke damage to be more accurately assessed and enable clots to be removed, stents to be placed, and other procedures to be performed via a blood vessel rather than by an open surgical procedure.
- Neurological/Neurosurgical intensive care units (neuro ICUs). Neuro ICUs are staffed by highly specialized physicians, nurses, and other clinical staff who have training and vast experience in caring for complex neurology and neurosurgical patients. These units provide immediate access to intubation and emergent brain decompression kits, and give 24/7 access to the specialized staff needed for life-threatening neurological emergencies. Almost 90% of the hospitals in the United States certified by the Joint Commission as Advanced Comprehensive Stroke Center Hospitals are teaching hospitals.1 This certification status requires a wide array of the most advanced personnel and technology resources to be available around the clock.
- Sophisticated electronic medical record (EMR) systems and protocols. America's teaching hospitals have been at the forefront in developing and implementing sophisticated EMRs and embedding evidence-based care protocols in them. For stroke patients, the EMR prompts might include reminders for use of the modified NIH Stroke Scale on each shift to check the patient’s neurological deficits and status, deep vein thrombosis prevention techniques, neuro-checks, repositioning to avoid pressure ulcers, lab draws to assure that anticoagulation drugs remain at safe blood levels, and catheter care.
- Timely access to specialized preventative and rehab expertise. Because of the size and medical complexity of their patient populations, teaching hospitals can provide extended access to clinical staff specialized in prevention and rehabilitation services. Accordingly, stroke patients — even when admitted on weekends — can be evaluated soon after admission by a speech pathologist or other professional trained to determine the risk of aspiration, a nutritionist to assure that the patients nutritional intake help prevent formation of pressure ulcers (a risk in stroke patients), and physical and occupational therapists to help assess deficits and begin to plan for rehabilitation.
Stroke is a major cause of death and disability among Americans. However, America’s teaching hospitals, through research, training of health professionals, and development and provision of the most advanced patient care strategies, continue to contribute to improvements in the number of lives saved after a stroke and the ability of patients to regain independence and thrive after a stroke.
1. AAMC analysis of 2018 Joint Commission data.