Nothing seemed out of the ordinary when Kimberly L. Reynolds, MD, greeted her new patient, a three-year-old girl, in the emergency department of a large pediatric hospital. The third-year resident introduced herself to the child’s parents, then bent down to talk with the girl.
That was when the father, calmly and quietly, asked Reynolds not to touch the child. He and his wife would prefer a different doctor, he told Reynolds, who has since left that hospital and is now assistant professor of clinical pediatrics at the University of Miami Miller School of Medicine. Uncertain of what she had heard, Reynolds asked why. “We would like a white doctor, please,” he said.
Reynolds took a few steps back. “It felt as if someone had punched me,” she said, recalling the incident that happened about four years ago. “I decided to exit the situation and try to process what was going on.”
“In medical school, an African American friend and I were routinely mistaken for a janitor or cleaning person.”
Altaf Saadi, MD
Massachusetts General Hospital and Brigham and Women’s Hospital
At most medical schools and teaching hospitals, cultural competency education is part of the curriculum to improve care, and reduce health inequities. But when it comes to addressing patient biases toward physicians, “you can’t give those modules to the public,” said Emily E. Whitgob, MD, MEd, a medical fellow in the Department of Pediatrics at the Stanford University Medical Center.
Overt, explicit bigotry against physicians as happened to Reynolds is not an everyday problem at teaching hospitals. But not uncommon is subtle discriminatory behavior—patients making remarks about a doctor’s race, ethnicity, or religion, for example.
Bigotry at any level compromises the health care environment, academic medicine leaders would agree. And as Reynolds attests, bigotry from patients is distressing to doctors.
Addressing patient bias
Whitgob is coauthor of a 2016 Academic Medicine study of Stanford pediatric faculty leaders that looked at how trainees and faculty might respond to discrimination. The study arose from an incident in which a patient asked an intern if the intern’s last name was Jewish. If so, he said, he didn’t want her to be his doctor because he was Palestinian. Whitgob, who supervised the intern, wanted to provide support but felt limited by having no training for such an event. When she presented the case to other doctors, they painfully shared their own experiences with bigotry from patients.

Bias toward a physician may also be based on a patient’s implicit assumptions. Altaf Saadi, MD, chief resident in neurology at Massachusetts General Hospital and Brigham and Women’s Hospital, is Muslim and ethnically Iraqi and Iranian. She wears a head scarf for religious reasons. One day, a patient demanded, in a disdainful tone, to know what foreign medical school Saadi had attended. “I’ve had people ask me that same question in a nice way—‘Where did you train?’— without accompanying it with an assumption that it must have been somewhere that is ‘less-than,’” she said. Saadi told the patient she graduated from Harvard Medical School. The patient remained silent from then on.
“It’s hard to know what aspect of your identity influences these more implicit comments,” said Saadi. “In medical school, an African American friend and I were routinely mistaken for a janitor or cleaning person.” The two friends began wearing white coats regularly to avoid such moments.
Saadi’s name, skin color or head scarf may well have influenced her patient’s negative questioning. A 2015 study of 255 Muslim physicians in the United States, conducted by a team from the University of Chicago, found that 24% had experienced frequent religious discrimination during their careers. Patients refused care from nearly 10% of those physicians, citing the physicians’ Muslim religion as the reason. The study appeared in AJOB Empirical Bioethics.
When discrimination happens
The issues involved in dealing with patient bias are complex. Patients have the right to refuse care from a physician if they are mentally competent and do not have an emergency condition. Some institutions may have policies related to disruptive patients that could apply when patients show bigoted behavior.
Before responding to patients’ biased actions, physicians often consider factors such as the patient’s medical condition, decision-making capacity, and reason for the discrimination. When bigotry is unequivocal, some doctors tough it out silently. Others may take problems to senior physicians. Reynolds, whose patient’s parent refused her care because she was African American, went to her attending, a white male. Without asking what she wanted to do, he told the parent Reynolds was competent and was going to examine the child. She then did.
Although appreciative of her attending’s action, later “I was kind of ashamed and sad,” said Reynolds. She didn’t talk about the incident much until co-authoring a 2015 Pediatrics article examining the ethical dilemmas posed by patient discrimination.
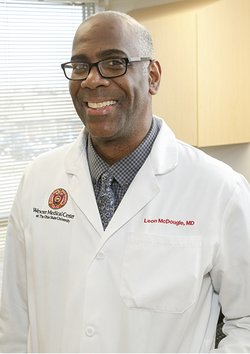
Leon McDougle, MD, MPH, chief diversity officer of The Ohio State University Wexner Medical Center was in a similar situation as an intern. McDougle was to deliver a baby but the expectant father objected because of McDougle’s race. His senior resident gave him a choice, to deliver the baby or not. McDougle wanted to do it, so the resident spoke to the couple and McDougle handled the delivery. “This is where leadership comes into play,” said McDougle, a past chair of the AAMC Group on Diversity and Inclusion. “How senior residents and faculty address these types of issues can really make a big impact.”
Training and guidelines needed
Although 12 of the 13 faculty members in the Stanford study had witnessed discrimination against a trainee and 8 had been personally discriminated against by a patient or family, only 4 had received formal training on how to respond. Almost all of those surveyed said faculty development was needed.
Their recommendations on dealing with discriminatory patients included assessing acuteness of illness (if the care needed is urgent or routine), trying to build a therapeutic alliance, depersonalizing the event, and providing support and assurance of competence to the targeted physician. Debriefing after an event is important as well.
Whitgob said dealing with bigoted patients should be discussed in the first year of medical school, before going into clinical settings, at the start of internship, and at every transitional step.
Reynolds wants professional guidelines developed about handling patient bias. “When you’re in a high-stress situation, which medicine is anyway, and you have the additional factor of being discriminated against, you develop a deer-in-the-headlights reaction—you don’t know what to do or where to turn,” she said. “I don’t think things are going to change and we might actually hear about more of these situations.”
As awareness grows about patient discrimination, said McDougle, institutions may look at approaches for faculty response and support. “This may very well be an opportunity to engage in a broader discussion and develop guidelines surrounding these sensitive issues,” he said.
